A comprehensive guide for people considering vasectomy
Vasectomy overview
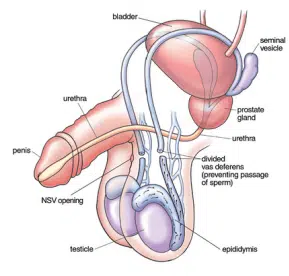
Vasectomy (male sterilisation or “the snip”) is a straightforward minor surgical procedure that permanently prevents pregnancy by cutting or sealing the tubes (vas deferens) that carry sperm. After a vasectomy, semen is still ejaculated during orgasm, but it no longer contains sperm.
It’s important to be sure about your decision before having a vasectomy, as it is intended to be a permanent form of male contraception. While reversals are sometimes possible, they are not always successful and should not be relied upon.
A vasectomy does not offer protection against sexually transmitted infections (STIs), so safe sex practices remain important.
Current medical guidelines recommend performing vasectomy under local anaesthetic. This means you’re awake but should not feel pain during the procedure, which typically takes around 15 minutes.
General anaesthetic is not routinely recommended for vasectomy, but it may be considered in cases of extreme anxiety or where surgery is more complex.
Overall, vasectomy is regarded as a safe, low-risk procedure with high satisfaction rates among men.
If you want to get the ball rolling (no PUN intended) then you can explore next steps and learn about our clinic, staff and services here – and if you want a vasectomy for free on the NHS click here for NHS vasectomy information
If you have a specific question, please look at the table of contents below, otherwise – happy browsing.
Vasectomy Terms in a Nutshell (Glossary)
Vasectomy is often referred to as “the snip” or “male snip.” You may also come across terms like “no-scalpel vasectomy” or “minimally invasive vasectomy.”
There are different techniques used, including open-ended and closed-ended vasectomy. Surgeons may seal the tubes using clips, sutures (stitches), or by relying on the body’s own tissue to create a natural block.
Below, we’ll explain these terms in more detail to help you understand the various options and what they mean for you.
Table of Contents
About the Author
Dr Kittel — Vasectomy Specialist

This page is designed to give you everything you need to know about vasectomy in one place — a kind of “vasectomy in a nutshell.” You’ll find links for further reading and quotes from evidence-based studies throughout.
I’ve written this based on over 20 years of experience as a vasectomy surgeon, specialising in minimally invasive no-scalpel techniques. Having performed more than 20,000 procedures, I’ve learned what matters most to patients — and what they wish they’d known beforehand.
How a vasectomy is carried out
Vasectomy is a quick and generally low-pain surgical procedure. In most cases, you’ll be able to go home the same day.
There are two main types of vasectomy:
Conventional vasectomy – performed using a scalpel (surgical knife)
No-scalpel vasectomy (NSV) – also known as
Minimally Invasive Vasectomy (MIV), a more modern technique that’s less widely known but increasingly used
Your doctor will explain which method they offer. However, clinical guidelines recommend
no-scalpel or minimally invasive vasectomy as the preferred technique due to its
lower risk of complications and quicker recovery time [2].
Vasectomy and No-Scalpel Vasectomy in Detail
Differences Between No-Scalpel (Minimally Invasive) and Conventional Vasectomy
Conventional Vasectomy:
Anaesthesia: Local anaesthetic numbs the scrotum.
Incisions: Two cuts are made on each side of the scrotum to access the vas deferens (sperm tubes).
Procedure: Each tube is cut, a small section is removed, and the ends are tied.
Stitches: The cuts are stitched, typically with dissolvable stitches or clips, which dissolve within three to six weeks.
Healing: Slightly longer healing time compared to No-Scalpel Vasectomy.
No-Scalpel Vasectomy (NSV) / Minimally Invasive Vasectomy (MIV):
Anaesthesia: Local anaesthetic numbs the scrotum.
Incisions: A tiny puncture hole is made in the scrotum, avoiding scalpel cuts.
Procedure: The tubes are cauterised, and an “open-ended method” may be used for the lower vas. The upper vas end is sealed with heat, radiofrequency cautery, or a stitch or clip to prevent sperm entry. A small piece of the vas deferens may be removed.
Stitches: No stitches required in the classic No-Scalpel method.
Healing: Less bleeding and quicker recovery with fewer complications.
If you’re interested in a no-scalpel vasectomy without clips or sutures, visit our website’s front page.
During the Procedure
Vasectomy surgery typically takes about 10 to 30 minutes, although you should expect to spend around 30-60 minutes at the clinic, including aftercare and some time to rest. During the procedure, your doctor will likely follow these steps:
Pre-procedure conversation:
The doctor will invite you into the treatment room and discuss any final concerns. The doctor and staff will introduce themselves.Preparation for surgery:
The doctor and staff will clean their hands, wear masks (some clinics may offer you a mask for infection prevention), and disinfect the area with a mild antiseptic.Securing the area:
The area will be draped, and the penis will be secured away from the surgical site to reduce the risk of injury.Numbing the area:
A local anaesthetic will be injected into the skin of your scrotum with a small needle to numb the surgery area.Accessing the vas deferens:
The doctor will make a small opening in the upper part of your scrotum once the area is numb. In the No-Scalpel Vasectomy (NSV) technique, this is typically a small puncture using a metal haemostat or electrosurgical equipment instead of a traditional incision.Working with the vas deferens:
The doctor will withdraw part of the vas deferens through the incision or puncture and then either interrupt or cauterise it. Some surgeons may remove a portion of the tube, while others may not. Various techniques are used, such as cauterising internally or externally, and some surgeons may use a clip or suture, while others may avoid foreign materials altogether.Repeating the procedure on the other side:
The same process will be repeated on the other side. In NSV, only one incision/puncture is typically used for both sides.Closing the wound:
After the procedure, the incision site will be closed. In conventional vasectomy, stitches or glue may be used. For No-Scalpel Vasectomy, the wound is typically so small that it heals on its own without the need for stitches. Some clinics may apply a silicone plaster to aid the healing process.
After Your Vasectomy (or the Snip) – Recovering After the Operation
Painkillers
It’s common to experience mild discomfort, swelling, and bruising of your scrotum for a few days after your vasectomy (or the snip). You can take painkillers like Paracetamol (or Acetaminophen in the US) to help manage any pain. If the pain persists after taking painkillers, consult a GP.
Underwear
Wear snug-fitting underwear day and night during the first few days following your vasectomy to support your scrotum and ease any discomfort or swelling. Be sure to change your underwear every day.
Hygiene
Avoid getting water on your wound for the first 48 hours after the snip. After that, it’s safe to shower, but avoid baths and swimming pools for about a week, as they can be contaminated. Click here for more information about postoperative hygiene.
Returning to Work
You can usually return to work 1 or 2 days after your vasectomy. However, avoid manual labour, sports, and heavy lifting for at least a week to prevent complications. If you continue to experience symptoms after a few days, consult a GP.
Having Sex
Treat sex like any other form of exercise, and avoid sexual activity for at least 7 days after your vasectomy. You’ll need to use an alternative form of contraception until the remaining sperm in your tubes clears. This process varies for each man. Your surgeon will let you know when you can schedule your first sperm test. During this time, there is still a risk of pregnancy. It’s also common to notice blood in your semen in the first few ejaculations after the snip, but this isn’t harmful.
Want to know more about sex after vasectomy – read this post
Summary of the Advantages and Disadvantages of Vasectomy
Advantages
A vasectomy (male snip) is more than 99% effective at preventing pregnancy.
It’s relatively inexpensive compared to most other forms of contraception, and in many countries, including the UK, vasectomy is funded by the NHS.
Long-term health effects are rare.
It doesn’t affect hormone levels, sex drive, or sexual pleasure.
You’ll still have normal erections and ejaculation, but your semen will no longer contain sperm.
It may be chosen as a simpler and safer alternative to female sterilisation.
It’s a permanent solution, so once it’s done, you no longer need to think about contraception.
Vasectomy is a highly sustainable form of contraception — it doesn’t pollute water with hormones, and it requires no ongoing supplies or appointments.
Want to hear real stories? Read our article: Good reasons for vasectomy – patient stories
Disadvantages
You’ll need to use contraception for at least 12 to 20 weeks after the procedure, as sperm may still be present in the tubes.
Vasectomy cannot be easily reversed, and reversals are rarely funded by the NHS.
You must continue using contraception until a semen test confirms you’re sperm-free.
Possible side effects include:
A haematoma (collection of blood in the scrotum)
Sperm granulomas (small lumps from leaking sperm)
Infection
Chronic testicular pain (rare but may require further treatment)
The vas deferens tubes can rarely reconnect, leading to failure of the procedure.
Vasectomy does not protect against sexually transmitted infections (STIs) — condoms may still be needed.
Frequently Asked Questions
Personal FAQs
1. Will I still ejaculate after the snip?
Yes — your semen will still look and feel the same, but it won’t contain sperm. Your body continues to produce semen and testosterone as normal.
2. Does having a vasectomy affect my sex life?
Not at all. Most men experience no change in sexual function, and many report feeling more relaxed knowing pregnancy is no longer a concern.
3. Can I reverse a vasectomy if I change my mind?
Reversals are technically possible but not always successful. They’re rarely funded by the NHS and are more complex and expensive than the original procedure, typically approximately 5-10 times more expensive than a private vasectomy.
4. Is the snip painful?
You may feel a pinch from the local anaesthetic, but most men describe the procedure as mildly uncomfortable at worst. Afterwards, some soreness is expected for a few days.
5. Will my partner notice a difference during sex?
No — vasectomy doesn’t change the sensation or appearance of semen. Some couples say intimacy even improves because there’s no longer worry about unplanned pregnancy.
Read many personal questions patients have asked us over the years. Yours may be listed?! →
Clinical FAQs
1. How effective is a vasectomy?
More than 99% effective when followed by a confirmed sperm-free (negative) semen test. Even a few dead sperm remaining are OK.
2. What are the risks of vasectomy?
Risks are low, but possible side effects include bruising, infection, or rarely, chronic testicular pain. Recanalisation (tubes rejoining) depends on the surgeon and the average is 1:80 in the UK. However, some surgeons have much lower re-canalisation rates, the author typically has rates of 1:800
3. How long should I wait to have sex again?
Avoid all sexual activity for at least 7 days. Use contraception until a semen analysis confirms there’s no sperm in your ejaculate.
4. How soon can I return to work?
Usually 1–2 days after the procedure, but avoid strenuous activity for about a week. This includes manual jobs with more than 5kg of lifting.
5. What is a semen analysis and why is it important?
It’s a test to confirm that no sperm remain in your semen. Without it, there’s still a risk of pregnancy — even if you feel recovered.
Want to read a lot more clinical questions patients regularly ask us →
How Much Should You Pay for a Vasectomy (or the Snip)?
The cost of a vasectomy (or the snip) can vary depending on where you live and the healthcare provider you choose. Below are approximate costs for the snip in different regions:
USA: Around $750
Western Europe: Around €650
UK: Around £600
It’s important to note that these prices may vary based on the clinic, the surgeon’s experience, and whether the procedure is carried out privately or through a public health system. Always check with the provider for an accurate quote before making a decision.
Look at our vasectomy fees if you are interested in our charges
How Will I Know If My Vasectomy (or the Snip) Has Worked? – Testing After Your Vasectomy
Delayed Protection
A vasectomy (or the snip) does not provide immediate protection against pregnancy. You will need to use an alternative form of contraception until your doctor confirms that there are no sperm in your semen. This typically takes several months, and you may need to ejaculate 30 times or more to clear any remaining sperm from your semen. Your doctor will discuss this in detail before and after your vasectomy.
Patience is a Virtue – Semen Sampling
In general, the longer you wait, the more likely you are to have a negative sample (i.e., no sperm present). Dr. Kittel has observed that a longer wait for semen sampling—around 20 weeks—appears to reduce the risk of late failure. He hypothesizes that early failures (which occur soon after the procedure) are sometimes mistaken for late failures, especially when semen sampling is conducted too early. Most services typically test 12-16 weeks after the snip. If you test too early, you might need to repeat the test, often at your own expense.
The Time for Sampling Has Come
When it’s time for your semen sample, your doctor will ask you to produce a sample by masturbating and ejaculating into a container. The semen will be examined under a microscope to check for the presence of sperm.
Stopping Additional Contraception
Once your semen tests free of sperm, your vasectomy is considered successful, and you can stop using additional contraception. However, some men may need more than one test. In certain cases, surgeons recommend two tests to confirm the vasectomy has been successful. Until it’s confirmed that your semen is sperm-free, continue using another form of contraception.
A Little Dead Sperm Doesn’t Make a Big Difference
Some men may have small amounts of dead sperm in their semen, but these sperm are immotile (unable to move) and are less likely to cause pregnancy. If this happens, your doctor will tailor their advice based on factors like the number of dead sperm and other medical considerations.
Vasectomy Failure
The testing process also helps identify the rare cases where the tubes (vas deferens) naturally rejoin themselves after the procedure. The chance of this happening is between 1 in 66 and 1 in 1000, depending on the technique used and the surgeon’s experience.
Late Vasectomy Failure
The risk of late failure (i.e., failing to prevent pregnancy after clearance) is very low, with an estimated occurrence of about 1 in 2000, according to a large UK-based audit study (1). This risk is higher if semen tests are done too early after the snip, as late healing can cause sperm to reappear after the patient has been given the all-clear. It appears the risk is lower when a service waits longer before confirming sterility and conducting semen testing.
How to Find a Good Vasectomy Service
Finding a vasectomy service that suits your needs is crucial for your peace of mind and long-term satisfaction. Here are some tips to help you choose the right surgeon and clinic:
Research the Surgeon
Start by exploring the surgeon’s website. Watch any videos they have created, and read through their content. Does the surgeon seem genuinely knowledgeable and experienced in performing vasectomy procedures? Experience matters—look for someone with a lot of practice and published results. Does the surgeon share their success rates, patient testimonials, or before-and-after results?Consider the Price
When it comes to a vasectomy, the price should be considered carefully. Like buying wine, cheaper options might not offer the same quality as a mid-range price. Be cautious with very low-priced services, as these might be less experienced or lacking in facilities. However, expensive services may not always be better, either. Surgeons who charge a premium often work in high-cost private hospitals and may not perform enough procedures to stay highly skilled.Examine the Technique and Care
Make sure the vasectomy service uses the latest techniques, such as No-Scalpel Vasectomy (NSV), which is known for having fewer complications and a quicker recovery time. Do they offer post-procedure support and clear guidance on recovery? A good service should offer a pre-procedure consultation to ensure you’re comfortable and well-informed.Consultation Opportunities
Feeling comfortable with your surgeon is key. Look for a service that provides the opportunity to speak with the surgeon or a nurse before the procedure, whether through a phone call or online meeting. This will help you feel confident and informed about your decision to undergo the snip.
How Long Will I Have to Wait for a Vasectomy?
The waiting time for a vasectomy can vary depending on whether you choose a private or NHS service:
Private Services
If you opt for a private vasectomy, many services can offer you an appointment within 1-3 weeks. If you encounter much longer waiting times, it could be a sign that the service is not well-managed or efficiently run.NHS Services
In many parts of the UK, a vasectomy is available free of charge through the NHS. However, waiting lists can sometimes be as long as 2 years, depending on your location. To check availability, speak to your GP or contact your local contraception clinic for more information about NHS vasectomies.Private vs NHS
Due to long waiting times for the snip on the NHS, some men opt to pay for a vasectomy privately to have the procedure carried out sooner. This can be a good option if you’re keen to get the procedure done without the wait.Experience of Surgeons
It’s worth noting that most doctors and surgeons who offer private vasectomy services often begin their careers in the NHS. This means that private vasectomy providers may have more experience due to the high volume of procedures they perform. Experience matters when it comes to ensuring a smooth and successful procedure. That said, a lot of NHS doctors are excellent surgeons.Specific Requests
If you have a preference for a doctor or surgeon of a specific gender, be aware that this may increase your waiting time, as the availability of specific practitioners may be limited.
Risks of Vasectomy
A vasectomy is generally a safe and effective procedure, but like any surgery, it comes with risks. Below are some potential risks and considerations to keep in mind:
Change of Mind
One of the major concerns associated with a vasectomy (or the snip) is the possibility of changing your mind later and deciding you want to father a child. While it may be possible to reverse a vasectomy, there are no guarantees it will work. Vasectomy reversal is more complicated than the original procedure, and success rates depend on factors such as the quality of the surgeon, the time elapsed since the procedure, and the age of the patient.
Vasectomy reversal is generally more expensive than a vasectomy, often costing up to 10 times more, but may still be the cheapest option compared to other fertility treatments.
Freezing sperm before the procedure is an option, though it’s limited in quantity and effectiveness. If frozen sperm is used for fertilisation, IVF (in vitro fertilisation) may be required, but this comes with its own challenges and expenses.
Other fertility treatments, such as IVF or ICSI (intracytoplasmic sperm injection), are also available, but these are typically expensive and not always successful. Sperm retrieval is another option, but finding a specialist for this can be difficult.
Common Early Side Effects
After a vasectomy, some men may experience mild to moderate side effects. These are usually short-term and resolve on their own, especially when performed by an experienced surgeon. Common early side effects (less than 5% risk with good surgeons and minimal major complications) can include:
Bleeding or blood clot (hematoma) inside the scrotum
Blood in your semen after the procedure
Bruising of the scrotum
Infection at the surgery site
Mild to moderate pain or discomfort
Swelling of the scrotum
The No-Scalpel Vasectomy (NSV) or Minimally Invasive Vasectomy (MIV) techniques are associated with fewer side effects, including less pain and quicker recovery times.
Delayed Complications
While complications are rare, some men may experience delayed side effects:
Chronic pain: Occurs in approximately 0.2-0.5% of men following a vasectomy. This condition is known as post-vasectomy pain syndrome (PVPS) and can sometimes require further treatment.
Vasectomy failure: In the rare case that a vasectomy fails, there is a chance of pregnancy. Before confirmation tests, the failure rate is approximately 1 in 500, but after confirmation, the rate drops to 1 in 2000.
Unfounded Concerns About the Male Snip
It’s completely natural to have concerns about having a vasectomy, often known as the snip. Many men worry it might cause serious health or sexual problems — but most of these concerns aren’t supported by evidence.
Here are some of the most common fears, and what research and clinical experience currently suggest:
Sexual Performance
Having the snip shouldn’t affect your sex drive or sense of masculinity. The procedure involves sealing the tubes that carry sperm (vas deferens), but it doesn’t alter hormone levels — your body continues to produce testosterone as normal. Most men report that their erections, sensation, and libido are unchanged after vasectomy. Some even say they feel more relaxed about sex, as they no longer need to worry about an unplanned pregnancy. That said, everyone is different, and how you feel emotionally or sexually afterward can vary.
Injury to Sexual Organs
While any surgical procedure carries some risks, serious injuries to the penis, testicles, or reproductive structures are considered very rare when the snip is performed by an experienced surgeon. In very uncommon cases, injury to the blood supply can result in the loss of a testicle — but this is an exceptional complication.
Cancer Risk
There has been past debate about a possible link between vasectomy and prostate or testicular cancer. However, large studies have not shown convincing evidence that the snip causes cancer. Most experts agree that if there is any risk, it is likely to be very small — and no causal relationship has been established. [Click here for more information]
Heart Disease
Similarly, earlier studies suggested a possible connection between the snip and heart disease, but more recent and higher-quality research has found no clear link. While this area of research continues, current medical opinion is that vasectomy does not increase the risk of heart problems.
Pain
Some men worry about pain during or after the snip, which is understandable. You may feel some pulling or mild discomfort during the procedure, despite the use of local anaesthetic. Afterward, it’s common to have soreness or swelling for a few days, but most men recover quickly. Long-term pain is rare, but can occur — often described as a dull ache or occasional sensitivity. If you’re concerned about pain, ask your doctor about the technique they use, as minimally invasive or no-scalpel methods tend to reduce these risks.
Further reading about vasectomy:
For Frequently Asked Questions about vasectomy
On a clinical level (facts): FAQ clinical
On a personal level (worries): FAQ personal
Patient stories: Good reasons for a no scalpel vasectomy
Reasons against vasectomy: Why not to get a vasectomy
References
(2) A comparative study of the no scalpel and standard incision approaches to vasectomy in 5 countries. The Male Sterilization Investigator Team
- Martin Kittel
- Most recent update: 15/07/2025
- 6:28 pm
- Page first published: 08/02/2025